Glaucoma Management & Surgery
Our glaucoma specialists have extensive training and expertise in determining the underlying cause of your glaucoma, and the best way to treat it.
We comprehensively manage glaucoma with medications, laser, cataract surgery for closed angle glaucoma, “cataract plus” procedures to reduce dependence on eye drops, trabeculectomy filtration surgery, and tube shunt surgery.
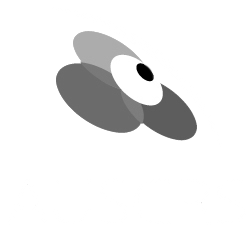
Glaucoma is a disease that involves damage to the optic nerve. The optic nerve head becomes cupped – an excavation of the central part of the nerve where nerve tissue has been lost. Cupping of the nerve leads to loss of peripheral, or side vision, which can impair many tasks. It can increase the risk of falls, and in some cases preclude driving.
In most cases people are not aware of the loss of vision in glaucoma, even if it is quite severe. It is therefore important to have checks to ensure that glaucoma is detected early before there is significant loss of vision.

Left image - Healthy Optic Nerve
Right image - Cupping of Optic Nerve
What are the types of glaucoma?
Traditionally glaucoma was thought of as a disease of high pressure. More recent research has confirmed that pressure is not the whole story. There are many people who develop glaucoma with pressures that are in the normal range, and others who have high pressures but do not develop glaucoma. There are a number of different factors that help a specialist to determine the risk of glaucoma either developing or progressing, and this risk assessment helps in the decision of whether or not treatment is required.
There are two main forms of glaucoma – open angle glaucoma and closed angle glaucoma. It is very important to distinguish between the two, as the treatment for each is very different. The only way to differentiate between these two is to look directly at the drainage angle with a mirrored lens: gonioscopy.
Visit Glaucoma Australia for more information about glaucoma and services available.

This visual field test shows an inferior defect in a classic pattern for glaucoma
How is open angle glaucoma treated?
Patients with open angle glaucoma have both damage to the optic nerve, and no blockage or closure of the main drainage area of fluid out of the eye.
The main treatment for glaucoma is to lower the eye pressure. Even if glaucoma develops with ‘normal’ pressures, studies show that reducing the eye pressure further reduces the change of ongoing vision loss.
Drops for glaucoma
One option to lower pressure is eye drops. These must be taken regularly every day to ensure the pressure stays low. There are a number of different eye drops and your specialist will help select the best one for you, in part based on any other health problems you may have.
Laser for glaucoma
An alternative to drops for lowering pressure is Selective Laser Trabeculoplasty (SLT). For many patients remembering to take drops can be difficult, or there may be side effects from the drops that are unpleasant. SLT is a good option, and around 80% of people will achieve an acceptable reduction of pressure following SLT.
Cataract surgery for glaucoma
Patients with open drainage angles may have a small reduction in pressure with cataract surgery, but it often wears off over time. There are a number of new surgical devices becoming available, that when combined with cataract surgery may help to lower the intraocular pressure, or make patients less reliant on drops.
Trabeculectomy for glaucoma
For patients whose pressure is still too high despite drops and laser, surgery may be required. Trabeculectomy involves creating a new drainage hole from inside the eye to allow the fluid outside the eye, being resorbed underneath the outer skin of the eye, the conjunctiva.
Tube surgery for glaucoma
In patients requiring surgery for glaucoma, insertion of a plastic tube into the eye is another option. It is generally used when there is a high risk of a trabeculectomy failing, or when a previous trabeculectomy has already failed.
How is closed angle glaucoma treated?
In patients with closed angle glaucoma, the drainage angle of the eye is closed over by the peripheral iris. While some patients may have a very high attack of pressure that needs a visit to an emergency department, more commonly, people have chronic angle closure and do not have any major symptoms. It is therefore important to have a check of the drainage angle to make sure that is remains open. A cataract is a clouding and enlargement of the natural lens of the eye, as this occurs, it contributes to progressive narrowing of the drainage angle.
Some people with narrow drainage angles do not need any treatment, other than a regular review to look at the drainage angles with a gonioscopy lens.
Laser peripheral iridotomy for glaucoma
Once more than half of the drainage angle has closed over, a number of studies suggest it is important to open the drainage angle. The most common method of doing this is a laser peripheral iridotomy. This involves making a small hole in the coloured part of the eye, the iris, which allows the pressure on either side of the iris to become the same. In most instances this prevents an acute attack of high pressure, and also reduces the chance patients will go on to develop chronic angle closure.
Cataract surgery for glaucoma
Performing cataract surgery, or removing the natural lens of the eye that has gone cloudy, is very good at opening narrow drainage angles. If you have a cataract that is diminishing your vision and narrow drainage angles, cataract surgery is a better option than laser peripheral iridotomy. In patients whose cataract is early and not causing visual problems, the decision to perform surgery is more complex, and is best discussed with your glaucoma specialist.
Drops for glaucoma
Sometimes the pressure starts to rise in patients with narrow angle glaucoma, even after their drainage angle has been opened. In this situation drops are a good option to control the pressure.
If you would like an assessment for glaucoma, please call our rooms or make an online enquiry.
MIRANDA
Suite 1
20-24 Gibbs Street
Miranda NSW 2228
02 9525 5190
Fax: 02 9525 0202
Directions and parking
BONDI JUNCTION
Park Place
Suite 606b, Level 6
3 Waverley Street
Bondi Junction NSW 2022
02 9387 4427
Fax: 02 9388 0139
Directions and parking
HURSTVILLE
Suite 12, Level 2
33 MacMahon Street
Hurstville NSW 2220
02 9579 4004
Fax: 02 9570 1377
Directions and parking
HOURS
Monday to Friday
8:30am until 5:00pm
FOR PATIENTS
FOR REFERRERS
© 2017- SYDNEY EYE SURGEONS